
2023
Assessing changes in spinal interneuronal dynamics as a biomarker of gait impairment in Parkinsonian mice
PI: Nick Au Yong, PhD, Neurosurgery (Emory); Co-PI: Chethan Pandarinath, PhD, BME (Emory/Georgia Tech)
Parkinson’s disease (PD) patients commonly experience gait disturbances, including early changes in gait cadence and speed, and also a severe manifestation known as Freezing of gait (FOG), which is poorly responsive to available treatments. Since the mammalian spinal cord contains the necessary circuitry to drive locomotor behaviors, PD-associated gait impairments including FOG may result from the under-recruitment of locomotor brainstem nuclei, reduced dopamine projections to the spinal cord, or both. Our team aims to investigate how dopaminergic neuronal loss in the brain affects the activity of spinal interneurons and motoneurons, crucial for locomotion, using a unilateral 6 hydroxydopamine (6-OHDA) lesion mouse model.

2023
Active learning to characterize the dynamics of deep brain stimulation local evoked potentials in a nonhuman primate progressive model of parkinsonism
PI: Annaelle Devergnas, PhD, (Emory Primate Center); Co-PI: Matthew Gombolay, PhD, Interactive Computing (Georgia Tech)
Deep brain stimulation (DBS) of the subthalamic nucleus (STN) has been a life-changing therapy by treating the motor symptoms of over 150,000 patients with Parkinson’s disease (PD). However, delivering the correct stimulation setting is critical to providing effective therapy. The standard approach is a tedious process of trial and error where the stimulator is programmed by a clinician while observing the patient. This process is subjective it can take many hours. The best solution would be an objective biomarker measured from the brain that could quickly determine if a stimulation setting will help a patient. A potential biomarker to optimize STN DBS is the STN DBS local evoked potential (DLEP). In this study we will record DLEPs in monkeys as they are progressively made parkinsonian. In parallel we will develop novel technologies for optimizing and controlling DLEP activity. Finally, we will validate our findings by comparing our data to a limited data set collected from patients.

2023
Modeling the effects of Parkinson’s Disease on free behavior and sensorimotor integration
PI: Eva Dyer, PhD, BME (Georgia Tech/Emory); Co-PI: Chris Rodgers, PhD, Biology (Emory)
Parkinson’s Disease (PD) is characterized by a prolonged period of neurodegeneration in the basal ganglia and accompanying gradual loss of motor function. Much less studied are its subtler sensorimotor and cognitive effects which arise from disordered neural circuitry distributed over the entire brain, including multiple regions of the cerebral cortex. A better understanding of how changes in this distributed neural circuitry lead to quantifiable changes in natural behavior would enable us to develop more targeted and precise therapies that target those circuits. In this project, we will apply our newly developed computational approach to understanding behavior at multiple timescales to discover the changes in behavioral style that accompany PD.

2023
Altruistic MSC-Based Mitochondrial Therapy for Parkinson’s Disease
PI: Melissa Kemp, PhD, BME (Georgia Tech/Emory); Co-PI: Levi Wood, PhD, ME (Georgia Tech)
Parkinson’s disease (PD) causes motor impairment, such as muscle rigidity, tremors and bradykinesia due to loss of dopaminergic (DA) neurons, leading to reduced dopamine and decreased stimulation of the motor cortex. There are currently no therapeutic interventions capable of preserving DA neurons. Although one of the key pathological hallmarks of PD is aggregation of α-synuclein protein, converging evidence from genome-wide studies and environmental factors supports that the primary cause of neuronal loss is failure of mitochondria, which is the powerhouse of the cell. Based on this evidence, the goal of the current proposal is to create a bioengineering-based cell therapy for Parkinson’s disease by treating disease-exposed DA neurons with mesenchymal stem cells (MSCs). MSCs are being explored for treating many age-associated diseases, and we have recently shown that they actively transfer their functional mitochondrial to other cell types. Based on these findings, our central hypothesis in the current study is that MSCs can be used to ‘implant’ healthy mitochondria into diseased DA neurons that will promote their survival and function.

2023
Developing new molecular tools to reveal the neurophysiological basis of Parkinson’s disease
PI: Jeffrey Markowitz, PhD, BME (Georgia Tech/Emory); Co-PI: Dorothy Koveal, PhD, BME (Georgia Tech/Emory)
Dopamine is known to play a critical role in everything from our capacity to learn to our ability to move. The loss of dopamine release in a specific part of the brain known as the basal ganglia is a hallmark of Parkinson’s disease, a disease that severely impacts nearly 6 million people worldwide. Understanding dopamine is therefore key for understanding the brain’s role in behavior and movement, and in treating Parkinson’s. However, despite its fundamental importance, the link between changes in dopamine concentration and changes in downstream neural activity remains unresolved. The primary objective of this proposal is to bridge this gap by developing robust optical tools for accurately measuring dopamine concentration and neural activity at the same time in freely moving animals.

2023
Non-motor signatures of disease progression in a mouse model of Parkinson’s disease
PI: Garrett Stanley, PhD, BME (Georgia Tech/Emory); Co-PI: Ellen Hess, PhD, Pharmacology & Chemical Biology/Neurology (Emory)
Most closely associated with Parkinson’s disease (PD) are the characteristic motor symptoms including stiffness and trembling, which are caused by a gradual decrease in the dopamine supply to the striatum. PD patients, however, also suffer from non-motor impairments including altered sense of audition, olfaction, and tactile perception (Richardson & Sussman, 2019; Haehner et al., 2010; Sathian et al., 1997). Non-motor deficits may play an underestimated role, especially in the disease’s early development, prior to classic motor symptoms. The cellular and circuit mechanisms of these impairments remain unknown, but previous esearch suggests that dopamine (DA) plays a crucial role in both motor and non-motor functioning (Reig & Silberg, 2014; Juri et al., 2009; Liljeholm & O’Doherty, 2012). The long-term goal of this project is to establish a model for the early diagnosis of PD, relying on distinct biomarkers. This project’s objective is to elucidate neuronal dysfunction underlying these deficits in PD and their consequences for behavior.

2023
Neuromechanical interactions between perceptual, cognitive, and motor deficits underlying balance impairments in Parkinson’s disease
PI: Lena Ting, PhD, BME (Emory/Georgia Tech); Co-PIs: Michael Borich, PhD, Rehabilitation Medicine (Emory); J. Lucas McKay, PhD, Biomedical
Informatics/Neurology (Emory); Stewart Factor, PhD, Neurology (Emory)
Fall risks is 5x greater individuals with Parkinson’s disease and postural instability is a cardinal sign of Parkinson’s disease (PD). But, falls cannot be considered a purely motor problem in PD. We know that balance impairments in PD are associated with poor sensory and cognitive function, yet we lack a scientific understanding of why these associations exist. As PD is a disease affecting brain network function, our objective is to identify brain and biomechanical mechanisms underlying perceptual-motor (Aim 1) and cognitive-motor (Aim 2) interactions that cause poor balance function in individuals with PD.

2023
Force-dependent interaction and mechano-regulation of microglial and neuronal cell receptors Mac-1 and Lag3 by α-synuclein in Parkinson’s disease
PI: Cheng Zhu, PhD, BME (Georgia Tech/Emory); Co-PI: Stephen Traynelis, PhD, Pharmacology (Emory)
Parkinson’s disease (PD) is the second-most common neurodegenerative disorder in the US with rapidly increasing cases annually as the population ages. While it causes motor dysfunction, the non-motor symptoms such as dementia are just as prevalent and burdensome, yet their mechanism is poorly understood and thus treatments are limited. A main feature of the non-motor symptoms is the accumulation of α-synuclein (α-syn), a protein that forms aggregates known as Lewy Bodies, which contribute to neuronal and microglial brain cell inflammation and death. As the resident immune cells of the brain, microglial cells in a healthy state remove over-accumulated α-syn aggregates. However, why and how the microglia are defective in clearing out α-syn aggregates, which become stiffer in PD, is poorly understood. Yet, α-syn binds receptors on the surface of microglial and neuronal cells such as Mac-1 and Lag3, respectively. We propose to characterize the forces of microglial and neuronal cells on Mac-1–α-syn and Lag3–α-syn bonds (Aim 1) and the impact of force on these bonds (Aim 2), using techniques unique to our lab but have not been used in PD studies. Our data would provide greater insight into the mechanism of PD and pave the way for future studies on potential treatment strategies of PD.

2022
MR-guided Concentric Tube Robot for Parkinson’s disease Deep Brain Stimulation
PI: Yue Chen, PhD, BME (Emory/Georgia Tech) Co-PIs: Deqiang Qiu, PhD, Radiology (Emory); John Oshinski, PhD, BME (Georgia Tech/Emory); Nicholas Boulis, PhD, Neurosurgery (Emory)
This team proposes to design, construct, and validate a robotic hardware and navigation system to accurately and safely perform MR-guided deep brain stimulation (DBS) procedures for Parkinson’s disease (PD) treatment. Our work is motivated by the prevalence of PD where 1 in 330 people has the disorder (about 1 million in the US alone), with 30% unresponsive to drug therapy. DBS is an effective approach and has been widely used in medically refractory patients. However, certain devastating complications such as inaccurate targeting and hemorrhaging can still occur in the current clinical procedures. This is primarily due to the lack of dexterous guiding mandrel and navigation system to accurately create a safe insertion path. The overarching goal of this project is to create a precise and dynamically steerable MR-guided needle robotic platform to enable accurate and safe DBS placement, coupled with a novel MR imaging protocol to localize the DBS targets and the blood vessels to identify a safe insertion trajectory. The successful completion of this project will provide us a pilot dataset both for preliminary characterization of variability of deep nuclei and for training our software, and a software tool that can be used in future studies to establish the relationship between stimulation site and clinical outcome.

2022
A Therapeutic Robotic Game system for People with Parkinson’s disease
PI: Charlie Kemp, PhD, BME (Emory/Georgia Tech) Co-P Madeleine Hackney, PhD, Geriatrics & Gerontology (Emory)
People with Parkinson’s disease (PD) have difficulty moving their bodies, including when they need to stretch to reach objects, quickly reach objects, and initiate body movements. People with PD also have difficulty with cognitive tasks, such as changing their actions for a new task and performing two tasks at the same time. This team proposes to develop a novel therapeutic robotic game system for people with PD to increase patient exercise quality, frequency, and duration, while reducing demands on overburdened therapists. The system will use a mobile robot that can safely reach space within a large volume around the player and a smart ball with sensors, sounds, and illumination. Their innovative research will make progress towards a future in which people with PD play fun therapeutic games at home with interactive robots, and therapists have more time to provide individualized guidance.

2022
Validation and clinical feasibility of a Speech-Assisting Multi-Microphone System for the treatment of communication deficits in people with Parkinson’s disease
PI: Amanda Gillespie, PhD, Otolaryngology (Emory); Co-PIs David Anderson, PhD, ECE (Georgia Tech); Adam Klein, MD., Otolaryngology (Emory)
Parkinson’s disease severely impacts communication in 70-90% of patients. Behavioral voice therapy can be effective in Parkinson’s-related voice and speech disorders by increasing vocal loudness and improving speech intelligibility. However, success in treatment is dependent on an intensive intervention schedule of four weekly sessions over four weeks duration with inter-session home practice. The long-term goal of this team’s research is to effectively reduce communication disorders in patients with PD. The objective of this project is to further refine and validate wearable personal technology that provides real-time feedback to address the most salient communication deficit in people with PD – reduced vocal loudness. Next steps include application for large scale funding to test the device as a component of behavioral voice and speech therapy for people with Parkinson’s Disease.

2022
Defining the causal role of brain activation to balance disorders in Parkinson’s disease
PI: Michael Borich, PhD., Rehabilitation Medicine (Emory); Co-PIs Lena Ting, PhD., BME(Georgia Tech/Emory); Lucas McKay, PhD, Biomedical Informatics (Emory)
Our long-term goal is to develop personalized, closed-loop, non-invasive brain stimulation techniques for targeting abnormal cognitive-motor interactions in Parkinson’s disease (PD) that lead to reduced mobility and falls. Here we propose to develop a state-dependent brain stimulation paradigm that uses time-locked electroencephalography (EEG) signals to trigger focal delivery of transcranial magnetic stimulation (TMS) to interfere with brain activity evoked by standing balance perturbations and measure the effects on brain activity and balance recovery in real-time. If successful, we will establish a novel state-dependent, open-loop stimulation paradigm to precisely measure and modulate functionally-relevant brain activity during standing balance control. Importantly, we will generate compelling preliminary data necessary to open a new line of discovery that will be supported by several externally-funded clinical and neurophysiological studies of PD pathophysiology and treatment. Support from the McCamish Parkinson’s Disease Innovation Program will foster successful development of leading- edge technologies of biologically-informed assessments and interventions of balance disorders in individuals with PD to be tested and validated in multiple planned NIH R01 submissions to generate sustained impact.

2022
On-Skin Wearable tVNS System with AI-Powered Motion Classification for PD Rehabilitation
PI: Minoru Shinohara, PhD, Biological Sciences (Georgia Tech) Co-PIs: Woon-Hong Yeo, PhD., Mechanical Engineering (Georgia Tech); Brian Magerko, PhD, School of Literature, Media & Communication (Georgia Tech); Milka Trajkova, PhD., School of Literature, Media & Communication (Georgia Tech)
Individuals with Parkinson’s disease (PD) suffer from motor symptoms like tremors, rigidity, slowness, smallness, and poor balance and coordination. Research has shown that vagus nerve stimulation (VNS) paired with rehabilitation facilitates motor recovery in stroke or spinal cord injury rats. The VNS protocol needs to be specific, including the application timing depending on the type of motion. We aim to develop an on-skin, wireless, and automated tVNS system that stimulates the human nerve during rehabilitation and facilitates motor improvement in PD. The system will classify the motion quality during dance therapy via markerless motion capture and an Artificial Intelligence (AI)-powered algorithm. Depending on the motion classification, it will apply a weak and brief tVNS at the outer ear. Our interdisciplinary team of scientists, engineers, and a clinical researcher will collaboratively develop a prototype. The prototype will be adaptable to various types of rehabilitation motions beyond dance.

2021
Striatal cell-type specific patterns of abnormal activity in L-DOPA-induced dyskinesias
PI: Ellen Hess, Pharmacology & Chemical Biology/Neurology (Emory); Co-PI: Chethan Pandarinath, Biomedical Engineering (Emory)
Parkinson’s disease is typically treated with L-DOPA. However, 80-90% of Parkinson’s disease patients develop L-DOPA-induced dyskinesias (LIDs) as a complication of long-term L-DOPA treatment. This team we will record striatal neuron activity in a model of LIDs and then apply recently-developed machine learning methods to identify specific patterns of neuronal activity that define LIDs.

2021
Developing improved deep brain stimulation designs employing real-time feedback methods to treat motor dysfunction in Parkinson’s disease
PI: Dieter Jaeger, Biology (Emory); Co-PI: Garrett Stanley, Biomedical Engineering (Georgia Tech)
The team is developing innovative deep brain stimulation methods to treat motor symptoms of Parkinson’s disease (PD). Specifically, they are engineering a closed-loop stimulation approach that continuously updates in real-time the parameters of electrical stimulation that feeds back into relevant brain areas to treat PD motor symptoms, based on recorded brain activity.

2021
Human activity recognition to track freezing of gait in Parkinson’s disease
PI: J. Lucas McKay, Biomedical Informatics/Neurology (Emory); Co-PIs: Gari Clifford, Biomedical Informatics/Biomedical Engineering (Emory), Stewart Factor, Neurology (Emory)
One of the most troubling and difficult to treat symptoms of Parkinson’s disease (PD) is Freezing of Gait (FOG). This study will use modern computer vision “human activity recognition” approaches to directly measure FOG in video recordings of PD patients with and without FOG collected and labeled by experts.

2021
Transcutaneous spinal cord stimulation for freezing of gait
PI: Svjetlana Miocinovic, Neurology (Emory); Co-PIs: Nicholas Au Yong, Neurology, (Emory), Stewart Factor, Neurology (Emory)
Freezing of gait (FOG) is a common symptom in patients with Parkinson’s disease (PD) where the ability to walk is abruptly interrupted, often described as if their feet were suddenly “glued” to the floor. This study will examine if lumbar transcutaneous spinal cord stimulation (tSCS), utilizing electrodes on the skin surface to deliver electrical stimulation to the spinal cord, can be used to improve walking and reduce or abort FOG episodes.

2021
Artificial intelligence dynamic network analysis for the multi-factorial and multi-scalar prediction of Parkinsonian disorders
PI: Cassie Mitchell, Biomedical Engineering (Georgia Tech); Co-PIs: Roman Grigoriev, Physics (Georgia Tech), Chao Zhang, Computational Science & Engineering (Georgia Tech), Chad Hales, Neurology (Emory)
The overall objective of this project is to differentiate and prioritize overlapping biomarkers of Parkinsonian disease; treatment targets; and patient risks, like medical history, environment, and lifestyle. The approach is state of the art data mining to construct a biomedical knowledge graph of multifactorial and multi-scalar relationships.

2021
Multimodel meta-optimization for the treatment of Parkinson’s disease
PI: Robert Gross, Neurology (Emory); Co-PI: Matthew Gombolay, Interactive Computing (Georgia Tech)
The combination of drug treatments and electrical brain stimulation is a life changing treatment for patients with Parkinson’s disease, as well as other neurological and psychiatric disorders. This team is developing a data-driven optimization algorithm that uses machine learning to quickly find the optimal stimulation parameters and medication dosage, using the same iterative process currently employed by clinicians – test, evaluate, and test a new parameter to find the best combination.

2021
Development and validation of personal technology for the treatment of communication deficits in people with Parkinson’s disease
PI: Amanda Gillespie, Otolaryngology (Emory); Co-PI: David Anderson, Electrical & Computer Engineering (Georgia Tech); Adam Klein, Otolaryngology (Emory)
Behavioral voice therapy can be effective in Parkinson’s-related voice and speech disorders by increasing vocal loudness and improving speech intelligibility. Clinical and market research demonstrate a dearth of, and need for patient-centered technology to improve communication in patients with Parkinson’s. This multi-disciplinary, multi-institutional team is developing the Speech-Assisting Multi-Microphone System (SAMMS), to isolate, monitor, and analyze vocal output for time and loudness and provide haptic biofeedback to the wearer.

2021
Wearable sensing and artificial intelligence to continuously examine acute and long-term measures of cardiovascular autonomic function in Parkinson’s disease and Multiple System Atrophy
PI: Omer Inan, Electrical and Computer Engineering (Georgia Tech); Co-PI: Chris Rozell, Electrical and Computer Engineering (Georgia Tech); Paul Beach, Neurology (Emory)
Dysfunction of the autonomic nervous system or dysautonomia, is common in Parkinson’s disease (PD) and a related condition called Multiple System Atrophy (MSA). Cardiovascular dysautonomia (CVD), such as impaired blood pressure response to standing, is especially associated with worse patient outcomes in both conditions. This team is developing novel wearable devices to allow non-invasive, continuous cardiac and blood pressure monitoring to afford an opportunity for easier assessment of CVD in both clinical (short-term) and real-world (at home/long-term) settings.
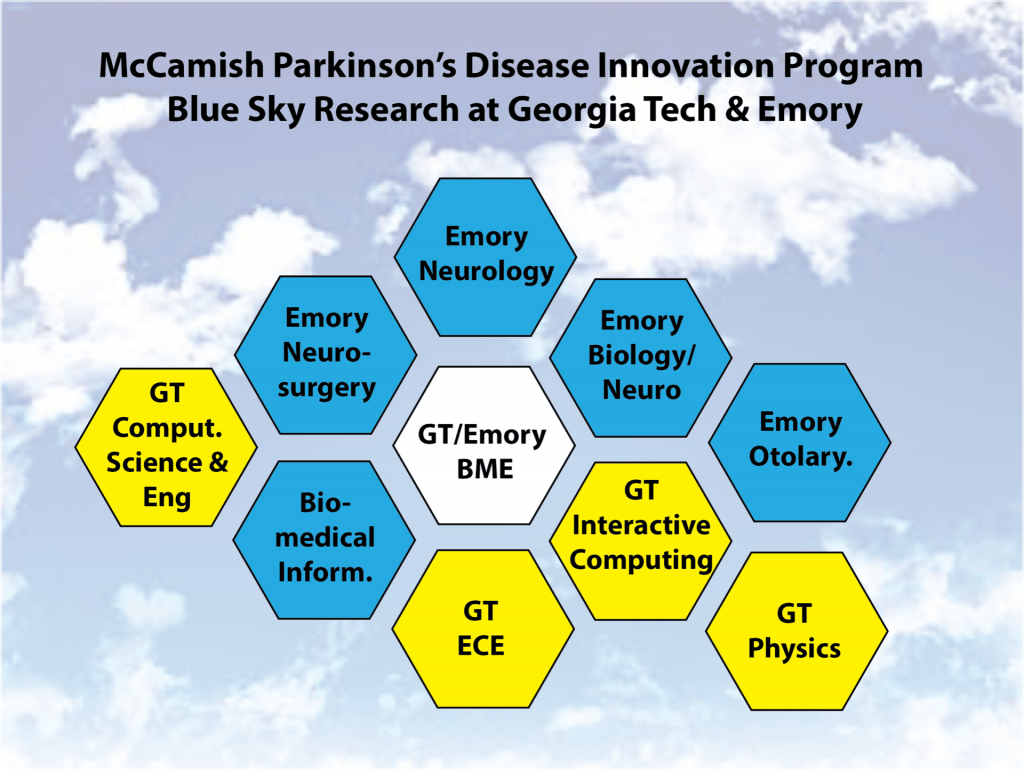 The McCamish Parkinson’s Disease Innovation Program supports a range of research projects at the interface of basic neuroscience, neuroengineering, data science and machine learning, and clinical neuroscience driven by diverse, collaborative teams across Georgia Tech and Emory University.
The McCamish Parkinson’s Disease Innovation Program supports a range of research projects at the interface of basic neuroscience, neuroengineering, data science and machine learning, and clinical neuroscience driven by diverse, collaborative teams across Georgia Tech and Emory University.